It is widely accepted that individuals should start paying closer attention to their health after turning 40. For women, this typically means beginning regular mammograms, while men are encouraged to monitor their prostate health. Over the following decade, screenings like colonoscopies become standard, leading to a continuous cycle of medical appointments and tests as one approaches their seventies or eighties.
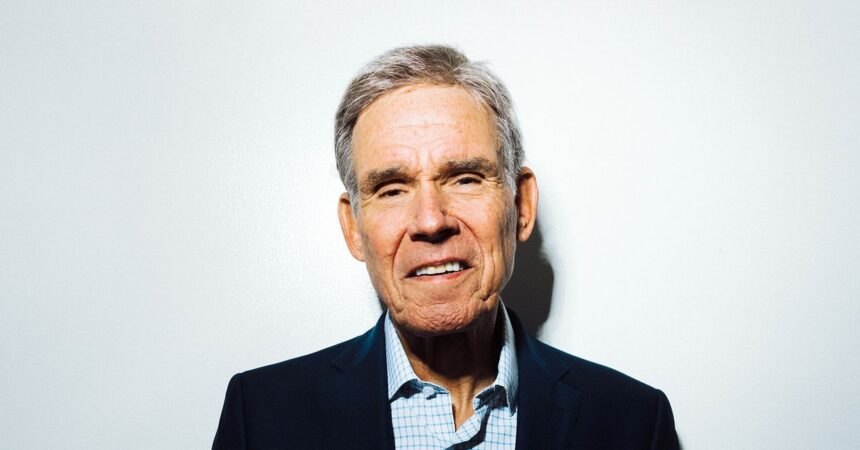
However, Dr. Eric Topol, a cardiologist, vice president of Scripps Research, and author of Super Agers, questions this conventional timeline. He argues that current medical practices may unnecessarily subject some middle-aged individuals to screenings for diseases they are unlikely to develop while neglecting younger populations who may have health vulnerabilities, such as an increased risk of colon cancer. He suggests there could be a more effective approach to maintaining health as we age—one that doesn’t require taking numerous medications daily.
During a recent discussion at WIRED’s Big Interview event in San Francisco, Topol shared insights gleaned while writing Super Agers. He highlighted an important distinction between “lifespan” and “health span,” asserting that neither is predominantly influenced by genetics. Evidence suggests that individuals classified as ‘wellderly’—those over 65 who are generally healthy—share a similar genetic makeup with those facing significant health challenges, such as heart disease and cancer.
Topol emphasizes the role of a robust immune system in promoting healthy aging. He advocates for a lifestyle that includes a diet low in ultra-processed foods, prioritizing sleep quality over mere quantity, and spending time in nature. Regular exercise is also essential; a balanced routine should incorporate aerobic activities as well as resistance and balance training, which can enhance resilience as one ages.
In his view, environmental factors should also be taken into consideration. Topol warns against exposure to stressors such as air pollution, microplastics, and harmful chemicals, all of which contribute to inflammation—an issue he believes remains inadequately addressed in current health policies.
According to Topol, the average American’s health span—the number of years one lives in good health—ranges from 63 to 65 years, contrasted with a lifespan of about 80 years. This indicates that many Americans may spend the final 15 years of their lives in a state of poor health. A statistic from the World Health Organization suggests that most seniors will experience just one “healthy birthday” beyond the age of 65.
“Health span should be extended as close as we can to lifespan, and I think we can do it,” Topol remarked during the event. He noted that we are currently at a pivotal moment in medicine, driven by advancements in AI and new data layers. Innovations such as organ clocks—tools that track aging rates across different body organs—and biomarkers like p-tau217, which can predict Alzheimer’s risk years in advance, signal significant progress in quantifying aging metrics.
Topol’s insights advocate for a re-evaluation of health maintenance strategies, particularly regarding age-related assessments and interventions.